What Is Neurally-Mediated Hypotension(OH)?
Orthostatic Hypotension (OH) means the blood pressure goes down when the person stands up and the person has orthostatic symptoms, such as dizziness, lightheadedness, changes in vision, and/or weakness.
A decrease in blood pressure with standing up can cause orthostatic symptoms but it can also make a person faint if the heart rate goes down.
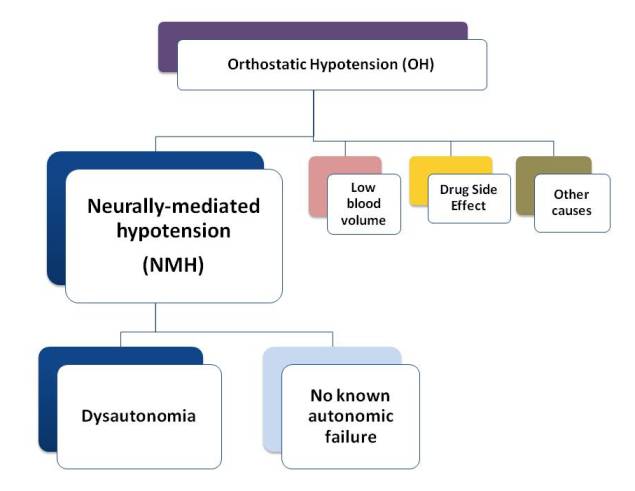
There are 4 main types or causes for OH and other causes related to specific conditions.
What is NMH
Orthostatic hypotension (OH) that is caused by a problem with the autonomic nervous system (ANS) is also called neurogenic orthostatic hypotension and neurally-mediated hypotension (NMH).
It is a chronic condition that can have significant effect on a person's daily life. It interferes with a person's ability to live a normal life2,3. It affects a person's ability to work, to go to school, do normal everyday life things (like have fun, go out to church, shop), and take care of themselves.
What is causing it?
It is caused by a problem with how the autonomic nervous system is functioning, how it is coordinating blood pressure and pulse messages between the blood vessels, the brain, the heart, the nerves and the endocrine organs. There has been damage to the nerves or the way they handle chemicals and hormones and send messages to the rest of the body organs. It is sometimes called autonomic dysfunction or dysautonomia.
The decrease in blood pressure with standing up is due to failure of the blood vessels to constrict (get narrower) when chemical messages are sent. (medical language - sympathetic vasoconstrictor failure).
With the decrease in blood pressure, there is a decrease in blood going to the brain and other organs starting at the top of the body. The person gets orthostatic intolerance symptoms: dizziness, lightheadedness, vision changes like black spots or tunnel vision, weakness.
The dysfunction may only be affecting the blood pressure/pulse system or it can be affecting other parts of the body that the autonomic nervous system controls.
The person may have a condition that is caused by autonomic failure, like Parkinson's, or a partial autonomic failure, like POTS. Or, there may not be any known failure of the autonomic system.
Fainting with NMH
With NMH, the blood pressure drops. If the pulse (heart rate) goes down also, the person will usually faint. When there is dizziness or fainting with the orthostatic drop in blood pressure, the person may go to the emergency room the first time (or other times if there is injury).
In people who first come to the ER, orthostatic blood pressure drop may be the cause of the symptoms in about 20% of the people with these symptoms in the ER. (If 100 people with these symptoms went to the ER, 20 of them would have OH)6
Difference in symptoms with OH
People with NMH have the usual orthostatic symptoms (dizziness, lightheadedness, vision changes, weakness), however, Medow and colleagues report that the people with OH do not report that they have the pallor, nausea/vomiting or clamminess (sweating).6
Other autonomic nervous system symptoms:
In NMH due to dysautonomia, other autonomic symptoms include; mild anemia, decrease sweating, sleep apnea, hoarseness, nasal stuffiness, constipation or diarrhea, Parkinsonian-like syndrome, recurrent urinary tract infections and/or bladder dysfunction, and impotence in men. For a full list of the other symptoms a person can have, check out Other Symptoms and Less Common Autonomic Symptoms.
Who Gets NMH?
NMH is the most common cause of recurrent fainting. (fainting more often)
Who gets NMH depends on what group of people are being studied or reported in an article.
What has been reported about NMH:
— There is a group of younger people who develop NMH, especially women.2
— It is common in people with low normal blood pressure.
— It is also more common following infection.
— It is more common in those with Chronic Fatigue Syndrome (CFS).
— Family members are often affected. In this group, the blood pressure lying down is often low.
The hypotension (low blood pressure) may not be detected (recorded) unless the orthostatic stress is prolonged (delayed OH). That means, a person has to continue to stand up, be still for a long period of time before the orthostatic changes happen. In a test situation like the Tilt Table, they do the test for 30-45 minutes or until the OH happens.
Which is more common - POTS or NMH?
In a review of children referred for autonomic testing, Sukul and colleagues found that POTS was the most common condition. It was found in in 71% of the chilcren.9 (If 100 children were tested, 71 would have POTS. If only 4 were tested, 3 would have POTS).
Orthostatic hypotension (NMH) was only present in 5%. (That would be 5 children out of 100 tested.)
For another perspective on the overlap between NMH and POTS, check out Types of OI under the Causes - Dysautonomia.
Can you have both - NMH and POTS?
Yes. It is possible to have both. One can occur when you first stand up. Then, if you keep standing up, the other can happen.
 Orthostatic Hypotension (OH):
Orthostatic Hypotension (OH):What is OH?
Criteria to diagnose OH
What is NMH?
OH due to low blood volume
OH due to drugs & other causes
Next Topics To Review
Causes of OI
Deconditioning
Getting Medical Care
Taking Care - Everyday Self-Care
References
- Moya, Guidelines for the diagnosis and management of syncope (version 2009). European Heart Journal (2009); 30: 2631-2671. Abstract. Article PDF.
- Freeman, Roy. Neurogenic orthostatic hypotension.NEJM 2008;358(6):615-624. Abstract
- Figueroa JJ, Basford JR, Low PA. Preventing and treating orthostatic hypotension: As easy as A, B, C. Cleve Clin J Med. 2010 May;77(5):298-306. Abstract. Article PDF.
- Wedro, Benjamin, Stoppler, Mellissa. Orthostatic hypotension. MedicineNet. Last accessed: June 24, 2012. Article"
- Brignole, M. The syndromes of orthostatic intolerance. E-journal of Cardiology Practice. 2007: 6(5). Access. http://www.escardio.org/communities/councils/ccp/e-journal/volume6/Pages/vol6n5.aspx
- Medow MS, Stewart JM, Sanyal S, Mumtaz A, Stca D and Frishman WH. Pathophysiology, Diagnosis, and Treatment of Orthostatic Hypotension and Vasovagal Syncope. Cardiology in Review 2008;16(1):4-20. Abstract.
- Winkelman, Chris RN, PhD, CCRN ACNP. Bed Rest in Health and Critical Illness: A Body Systems Approach. AACN Advanced Critical Care: 2009; 20(3); 254-266. Abstract.
- Brignole M. Diagnosis and Treatment of Syncope. Heart 2007: 93; 130-136. Article PDF
- Sukul D, Chelimsky TC, Chelimsky G. Pediatric autonomic testing: retrospective review of a large series.Clin Pediatr (Phila). 2012 Jan;51(1):17-22. doi: 10.1177/0009922811415102. Epub 2011 Aug 25. Abstract.
Author: Kay E. Jewell, MD
Page Last Updated: September 9, 2012
