What is POTS?
(Postural Orthostatic Tachycardia Syndrome)
Having POTS means a person gets orthostatic symptoms (dizziness, lightheadedness, weakness, headache, short of breath) when they stand up. The symptoms start anywhere from 2 to 10 minutes after standing up. The heart rate increases by 30 beats per minute or goes over 120 beats per minute.
People with POTS often have similar symptoms and ways it affects them and their lives, but not every one is the same. The cause of POTS is considered complex from a medical perspective. It can have different things causing it. Sometimes more than one thing can be happening in the body at the same time.
Other names for POTS: hyperadrenergic orthostatic hypotension, sympathotonic orthostatic tachycardia and idiopathic hypovolemia.
Symptoms: POTS is one of the conditions that causes orthostatic intolerance symptoms. Some of the more common symptoms in adults with POTS are lightheadedness, nausea, decreased concentration, tremulousness, palpitations, fainting and near fainting, fatigue and intolerance for exercise.8,9
In adolescents, the symptoms can go from mild dizziness to severe, autonomic dysfunction.8
There is a more complete list of symptoms here - Symptoms of OI.
Impact on a person's daily life: POTS can have a major effect on a person's daily life, interfering with the ability to go to school or work, to do daily activities outside the home like grocery shop, and daily activities of self-care like cooking, bathing, and walking around the house.
The level of impact on a person's daily function has been reported to be as severe as that experienced by people with congestive heart failure and chronic obstructive pulmonary disease (COPD).11 Despite this fact, they are often mis-diagnosed as having severe anxiety or panic disorders.9
In a study that looked at the quality of life of people with POTS, Benrud-Larson and colleagues reported the following:
"The average patient with POTS is a young, highly educated, previously healthy woman (mean age was 34 years in this sample), who should be facing many years of economic and social productivity."
Approximately 25% of the people were disabled and unable to work because of POTS.
"This figure is especially noteworthy given that younger age and more education are often associated with less disability among patients with chronic medical conditions.13 Clearly, the potential economic burden of POTS is great, both in direct costs related to health care and in indirect costs related to disability."
- How it starts
- Who gets it
- How common Is it
- Changes in the body with POTS
![]() For about 12% (12 out of 100 people with POTS) - the POTS symptoms come on quickly (acutely). 6
For about 12% (12 out of 100 people with POTS) - the POTS symptoms come on quickly (acutely). 6
![]() For about 14%, the symptoms develop over 1-3 months.6
For about 14%, the symptoms develop over 1-3 months.6
![]() For 6%, it comes on real slowly and is barely noticed when it started.6
For 6%, it comes on real slowly and is barely noticed when it started.6
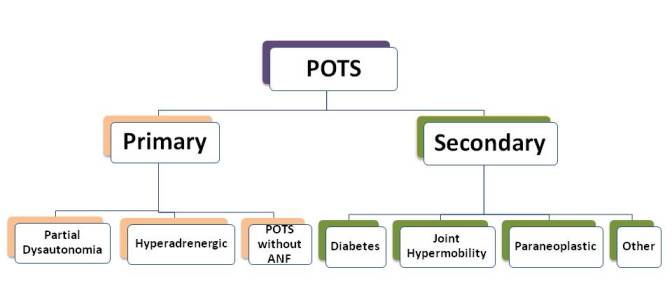
As the Primary Condition
When a condition develops in a person who has been healthy, it is called 'primary'. Example: A cold is a primary condition. If you get bronchitis after the cold starts, the bronchitis would be a 'secondary' condition that developed and was directly related to having a cold. POTS as a primary condition can start after a number of events.It is still primary because these conditions are not directly related to causing the POTS.
- After a viral infection - usually one that is longer-lasting than a cold.8
- Pregnancy
- After being immunized
- After surgery
- After trauma, like a traumatic brain injury (concussion) or other events like a car accident
- Sepsis - a severe, whole body infection
In the Mayo clinic experience, in the people who had some kind of an event before the POTS started, 90% of them had a viral infection. Surgery was the event in 10% of the people.6
![]() POTS in adolescents begins within 1-3 years of the growth spurt after a time of inactivity from an injury or illness. They find they cannot return to normal activities because of orthostatic symptoms when they stand up.8
POTS in adolescents begins within 1-3 years of the growth spurt after a time of inactivity from an injury or illness. They find they cannot return to normal activities because of orthostatic symptoms when they stand up.8
POTS as a Secondary Condition
POTS can develop when a person has another condition. An example would be a primary condition that causes damage to the autonomic nervous system, like diabetes. In this case, the POTS is called "secondary" POTS.
There is more information about the cause of POTS and secondary conditions here - see
Conditions that are associated with POTS
There are some conditions that the data shows happen more often in people who get POTS. It is not known if or what the connection is between them. Conditions that are associated with POTS include joint hypermobility syndrome (JHS) or Ehlers-Danlos Syndrome.
POTS affects women more than men- 5 to 1. That means 5 times more women get POTS than men. If there are 6 people with POTS, 5 would be women, one would be a man.
The majority of the people are Caucasian8
It is more common in individual with hypermobility as well as Ehlers-Danlos Syndrome.12,13
In adults, the age when most develop POTS is age 30. Most people with POTS are between 15 and 50 years. Most of the patients had symptoms for about 1 year before they were seen in the Mayo Clinic..7
Adolescents:They tend to be high-achieving individuals, successful in school and extracurricular activities.8 They also found hypermobility.
• POTS is the most common reason adults with orthostatic intolerance are referred.14
• Neurogenic orthostatic hypotension (NMH) due to autonomic neuropathies and non-autonomic
conditions are better known but they are not as common.
• How many people have POTS at any one time is not really known7.
• In 2008, it was estimated that there were at least 500,00 people with POTS in the US.10
• 25% of the people with POTS were disabled and unable to work. 11
• There have not been studies that look at the number of people with the diagnosis and how people
are doing after 5-10 years.
• Studies are needed that look at how many still meet the diagnosis of POTS, how many still have orthostatic
intolerance or symptoms with standing even if they no longer have meet criteria, how much the
orthostatic symptoms (intolerance) affect their daily life, how many are able to work/go to school, have a social
life and be physically active.
• The information that is available comes from clinics and clinicians who have specialized in diagnosing and
caring for people with POTS.
Some of the changes, such as tachycardia are also associated with people who are deconditioned, like people who have had prolonged bed rest7. There can be a longer recovery period than people without POTS have. They may have low energy even when they are resting. This sense of fatigue can occur in cycles, it may last for days or weeks and then be gone.
References
- Grubb, Blair P. Neurocardiogenic Syncope and Related Disorders of Orthostatic Intolerance. Circulation 2005; 111: 2997-3006. Abstract. Article PDF.
- Stewart JM. Chronic orthostatic intolerance and the postural tachycardia syndrome (POTS). J Pediatr. 2004;145:725–730. Article PDF
- Stewart JM, Medow MS, Alejos JC. Orthostatic Intolerance. Medscape article.
- Jacob G, Costa F, Shannon JR, Robertson RM et al. The Neuropathic Postural Tachycardia Syndrome. N Engl J Med 2000;343: 1008-14.
- Sandroni P, Opfer-Gehrking TL, McPhee BR, Low PA. Postural tachycardia syndrome: Clinical features and follow-up study. Mayo Clin Proc. 1999;74:1106–1110. Article pdf
- Thieben MJ, Sandroni P, Sletten DM, et al. Postural orthostatic tachycardia syndrome: The Mayo Clinic experience. Mayo Clin Proc. 2007;82:308–313
- Low PA, Sandroni P, Joyner and Shen W. Postural Tachycardia Syndrome (POTS). J Cardopvasc Electrophysiology 2009; 20:352-358. Abstract. Article PDF
- Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ and Fischer PR. Postural Orthostatic Tachycardia Syndrome: A Clinical Review. Pediatr Neuro 2010; 42:77-85. Abstract.
- Grubb BP. Postural tachycardia syndrome. Circulation. 2008;117:2814–2817. Abstract.Article PDF.
- Goldstein D, Robertson D, Esler M, Straus S, Eisenhofer G. Dysautonomias: clinical disorders of the autonomic nervous System. Ann Intern Med. 2002;137:753–763. Abstract.
- Benrud-Larson LM, Dewar MS, Sandroni P, et al. Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc 2002;77:531-7. Abstract. Article PDF.
- Rowe PC, Barron DF, Calkins H, et al. Orthostatic intolerance and chronic fatigue syndrome associated with Ehlers-Danlos syndrome. J Pediatr 1999;135:494-9. Article PDF.
- Gazit Y, Nahir AM, Grahame R, Jacob G. Dysautonomia in the joint hypermobility syndrome. Am J Med 2003;115:33-40. Abstract.Article
- Stewart JM, Weldon A. Vascular perturbations in the chronic orthostatic intolerance of the postural orthostatic tachycardia syndrome. J Appl Physiol 89:1505-1512, 2000. Abstract. Article PDF.
Author: Kay E. Jewell, MD
Page Last Updated: September 13, 2012
