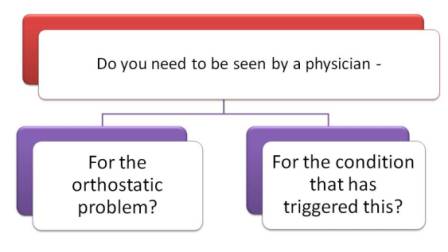
Do your orthostatic symptoms need physician evaluation or treatment - NOW?
The first question is to decide how severe things are, whether they need quicker more intense action or whether you can manage them at home.
If you have a primary physician who is familiar with your situation and managing flare-ups, this would be a good time to give them a call and explain the situation.
If that isn't an option that works right now, walk through these questions to see what you should do.
 How bad is your orthostatic problem?
How bad is your orthostatic problem?
You are the one who will have to decide if you need to see a physician for this now. These are questions that help you sort out how you are and help you make that decision.
When you answer these questions, you should be comparing how you feel now to what your normal is like.
Examples of what your "normal" might be when you stand for 2-3 minutes - it includes your symptoms:
• If you can only stand for 2 minutes usually without symptoms, then that is what you compare your answers to.
• If you have POTS, your BP usually stays the same & your pulse is less than 90 when you stand up, on meds.
• If you have NMH, your blood pressure usually drops 5-10 mmHg when you stand up & pulse stays the same.
How are you "right now"?
- Can you stand up for 2 minutes without fainting or collapsing or having to sit down? (Is that ‘normal’ for you?)
- Can you stand up to walk to the bathroom? Or is it so bad you can't stand up even 1 minute? Do you need to crawl to the bathroom?
- Do you have muscle twitches (that you usually don’t get)?
- Do you have more "brain fog" or confusion than usual? More trouble with words? Are you confused about people or things around you, a new confusion or confusion about the day or month?
- Have you ever been this bad before? What happened the other time(s)? Did you have to go to the ER or doctor to get fluids?
![]() If you answered yes to these questions, you might want to be evaluated by a physician or the ER. If you think you will need IV fluids, the ER is often the only option. Most doctor's offices do not have nurses on duty who can give IV fluids. An exception might be a special clinic like oncology.
If you answered yes to these questions, you might want to be evaluated by a physician or the ER. If you think you will need IV fluids, the ER is often the only option. Most doctor's offices do not have nurses on duty who can give IV fluids. An exception might be a special clinic like oncology.
If you're still not sure - other information that might help you decide
If you have a blood pressure cuff:
- What is your blood pressure and pulse when you lie down and then when you stand up – after 2 minutes?
- Does the top number of your blood pressure (systolic) standing up drop more than 20 mmHg?
- If you have neurally-mediated hypotension (NMH) or orthostatic hypotension,
- How much does your blood pressure drop"normally" when you stand up?
- Does it go even lower today? Do you have more symptoms? What is your pulse doing when you stand up?
- Can’t hear the heart beat for the top number? Or the cuff keeps saying “error” If you usually do your BP but you can’t hear it when you stand up – or your automatic BP cuff keeps saying “error”, then your BP is low.
- If your top number is under 90, it is definitely low!
Changes in your pulse (heart beat) when you stand up
What happens to your pulse when you are standing up for 1-2 minutes?
If you have NMH or orthostatic hypotension
- If your BP goes down and your pulse also goes down, especially below 50, it can trigger fainting.
- Is the change in your pulse now what usually happens for you?
- Does your pulse go up today? Is it more than 20 beats? (When the blood pressure goes down and the pulse goes up instead of down, it can mean the body is low on fluids).
If you have POTS
- Does your pulse go up way more than 30 beats?
- If you have been under pretty good control, does it go up more than it usually does when you check it?
- For example: if it usually goes up to 110 or 120 when your medication has worn off and now it's 130 or 140. What kind of symptoms are you getting when you stand up? If it is usually 90 or less with your medication and now it’s 110, that would be a difference.
![]() If you answered "yes" to these questions, you need to be evaluated for IV fluids. Contact your physician. This type of problem usually cannot be managed in the office unless they have a nurse who can do IVs. If it is after clinic hours, consider a visit to the ER for evaluation and IV fluids.
If you answered "yes" to these questions, you need to be evaluated for IV fluids. Contact your physician. This type of problem usually cannot be managed in the office unless they have a nurse who can do IVs. If it is after clinic hours, consider a visit to the ER for evaluation and IV fluids.

Even if you get IV fluids and they help, sometimes it takes the body 24-48 hours to readjust to the fluids.
 Does whatever is triggering the flare-up need to be evaluated (treated) by a physician or the ER - NOW?
Does whatever is triggering the flare-up need to be evaluated (treated) by a physician or the ER - NOW?
References
- Figueroa JJ, Basford JR, Low PA. Preventing and treating orthostatic hypotension: As easy as A, B, C. Cleve Clin J Med. 2010 May;77(5):298-306. Abstract --- Article PDF
- Rowe, Peter. General Information Brochure on Orthostatic Intolerance and Its Treatment. June 2010. Accessed from http://www.cfids.org/webinar/cfsinfo2010.pdf. Accessed May 28.2012.
- Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ and Fischer PR. Postural Orthostatic Tachycardia Syndrome: A Clinical Review. Pediatr Neuro 2010; 42:77-85. Abstract.
Author: Kay E. Jewell, MD
Page Last Updated: September 7, 2012
