Medical Care for OI
CFS-Orthostatic Intolerance is Common
Many people with CFS have symptoms of orthostatic intolerance – dizziness, vision changes, headache with standing, nausea & fatigue. It is one of the problems that can be managed and improve a person's daily life.1 The challenge with CFS is that the condition and its causes are not completely understood. It is likely there is more than one problem or cause of the symptoms and the whole condition. Orthostatic intolerance and the changes in the body that come with that, e.g. the low blood volume, decreased heart output, are just one part of the picture. But, there are things that can be done to address this part of the syndrome.
In the CDC website discussion of CFS , the section on management addresses the need to treat the most disruptive symptoms first.2
Recommendations are treatment of the conditions that are a priority for the patient
• Fatigue
• Sleep
• Pain
• Memory and concentration problems
• Depression, anxiety and distress
• Dizziness and light-headedness
In the CFS Primer released in May 2012, CFS/ME is described as a multisystem dysregulation with autonomic symptoms one of the 5 systems affected.3 Orthostatic intolerance due to POTS or NMH are cited as part of the diagnostic criteria and treatable problems.
Despite how common it is – and treatable - the other problems, like sleep and pain, often take priority when it comes to a doctor visit, for both the patient and the doctor. This may be something that needs to be reconsidered.
There is a potential advantage to paying more attention to orthostatic intolerance. Many symptoms of CFS are similar to symptoms of orthostatic intolerance. Treating the orthostatic problem could reduce the overall symptoms.
People with CFS can have POTS, NMH, syncope alone and they can have combinations of the conditions.
- In 1995, Bou-Holaigah and colleagues first reported that almost all of the people with CFS had OI. 4
- They reported that 96% of the patients (adolescents and adults) had neurally mediated hypotension (NMH) during a three stage upright tilt table test. Of these 70% had NMH in the first 45 minutes (Stage 1) of upright tilt. Of those who had NMH, 22% also had POTS.
- Studies since then have confirmed that orthostatic intolerance is common in pediatric CFS. They do not all have the same results. The number of people with NMH and POTS are different depending on the year the study was done, how they measured the NMH and POTS, by the patients seen and other factors.
- Early adult studies confirmed higher numbers of NMH in CFS patients than in controls (people without CFS). More recent studies with adult have generally confirmed higher rates of POTS.
- Hoad et al reported that 27% of the people with CFS met criteria for POTS. 5
- However, they acknowledge the number may be higher because they limited their testing to 2 minutes of standing time, not the current standard of 10 minutes.5
- People were found to have an increase in fatigue in those people whose heart rate increased within 30 seconds of standing.
- In one study, as many of 25-50% of adult patients with chronic fatigue syndrome had evidence of autonomic dysfunction, including POTS.6
- In the fludrocortisone randomized trial, Rowe and colleagues reported that 62% of patients with CFS had NMH, plus 4% had POTS. There was a total of 66% with OI.7
- Some cite as many as 90% of people with CFS have orthostatic symptoms.1
There are numerous studies that have reported on symptoms of autonomic dysfunction that are common in many people with CFS.21
The most common autonomic symptoms are: orthostatic intolerance, vasomotor symptoms (blood vessels), secretomotor, GI symptoms, sleep, and changes in how the pupils of the eye work. For more of the autonomic symptoms with OI, go to Delayed & Autonomic Symptoms of OI
Symptoms and patterns of orthostatic heart rate and blood pressure change in OTS overlap strongly with those of CFS.
Similar changes in the body in people with CFS and POTS. In medical terms, Stewart and colleagues reported12, 13
- loss of heart rate variability consistent with vagal withdrawal,
- increased blood pressure variability consistent with enhanced modulation of sympathetic tone while supine, and
- impaired baroreflex with a phase shift causing wide blood pressure swings uncompensated by compensatory heart rate changes.12
Orthostatic intolerance in POTS may represent a less intense form of chronic fatigue pathophysiology. Stewart 1999 Patterns However, the symptoms and patterns are more severe in those with CFS compared to those with POTS. Oko, stewart patterns
Drugs, like methylphenindate and dexamphetamine, that are recommended for fatigue in CFS are also effective in POTS and NMH.9
Physical findings - CFS and POTS
Physical findings that have been documented in people with POTS and in separate studies of people with CFS:
• decreased blood volume,( lower in CFS-POTS than just POTS11, 15
• small heart, and
• decreased stroke volume/cardiac output.
Like all conditions, not every person with CFS has these physical findings. Not all people with POTS have a small heart or left ventricle or other autonomic problems.
Looking at it from the other direction, some looked at the people with POTS to see how many also met criteria for a diagnosis of CFS11:
- 64% of those with POTS also met the criteria for CFS - in Okamoto's data.
- Okamoto reported the following:
- Others reported that 17-23 % of people with POTS also met criteria for CFS (not even 1 out of every 4 people with POTS)
- Fatigue was reported by one half to three fourths of people with POTS (48-77% of people with POTS)
Differences in the numbers could be because of how the information was collected (by questionnaire or chart review) and by the type of patients in the clinical group, whether the clinic is a primary clinic or a tertiary center that tends to see people with more severe POTS.
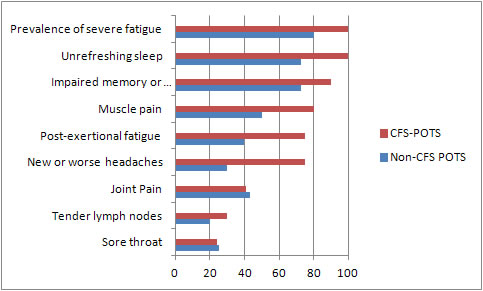
Okamoto reported the following differences in symptoms based on the CDC criteria for CFS11:
The Difference in Fatigue:
Almost all of the people (80%) who had POTS but did NOT have CFS had fatigue but their fatigue was different:11
• The fatigue was lifelong in 82% of the people.
• It was mainly related to exercise – 53%
.
• It was not disability 29%
.
• It had been there less than 6 months.
CFS differences that need to be addressed in management of orthostatic intolerance:
• Higher markers for sympathetic activity11, 16-20
• Inflammation - oxidative stress
• Post – Exertional Malaise
• More prolonged bed rest with subsequent deconditioning.
References
- Costigan A, Elliott C, McDonald C, Newton JL.Orthostatic symptoms predict functional capacity in chronic fatigue syndrome: implications for management. QJM. 2010 Aug;103(8):589-95. Epub 2010 Jun 9. Abstract. Article PDF
- CDC. Chronic Fatigue Syndrome. Treating the Most Disruptive Symptoms First. http://www.cdc.gov/cfs/management/treating-symptoms.html Last accessed August 23, 2012.
- .IACFS/ME Fred Friedberg, Bateman L, Begested A, Davenport T, et al. Chronic Fatigue Sydrome Myalgic Encephalomyelitis: A Primer for Clinical Practitioners.May 2012. Last Accessed 07.31.2012. Primer PDF
- Bou-Holaigah I, Rowe PC, Kan J, Calkins H. The relationship between neurally mediated hypotension and the chronic fatigue syndrome. JAMA. 1995;274:961–967. Abstract.
- Hoad A, Spickett G, Elliott J, Newton J. Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome. Q J Med 2008; 101:961–965. Abstract. Article PDF.
- Freeman R, Komaroff AL. Does the chronic fatigue syndrome involve the autonomic nervous system? Am J Med 1997;102:357-64.
- Rowe PC , Calkins H , DeBusk K , et al. Fludrocortisone acetate to treat neurally mediated hypotension in chronic fatigue syndrome (a randomized controlled trial). JAMA. 2001;285:52–59
- Wyller VB, Godang K, Morkrid L, Saul JP, Thaulow E, Walloe L. Abnormal thermoregulatory responses in adolescents with chronic fatigue syndrome: Relation to clinical symptoms. Pediatrics 2007;120:e129-37.
- Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ and Fischer PR. Postural Orthostatic Tachycardia Syndrome: A Clinical Review. Pediatr Neuro 2010; 42:77-85. Abstract.
- Stewart JM. Autonomic nervous system dysfunction in adolescents with postural orthostatic tachycardia syndrome and chronic fatigue syndrome is characterized by attenuated vagal baroreflex and potentiated sympathetic vasomotion. Pediatr Res. 2000 Aug;48(2):218-26. Abstract.
- Okamoto LE, Raj SR, Peltier A, et al Neurohumoral and haemodynamic profile in postural tachycardia and chronic fatigue syndromes. Clin Sci (Lond). 2012 Feb;122(4):183-92. doi: 10.1042/CS20110200. Abstract.Article PDF
- Stewart JM, Weldon A. Vascular perturbations in the chronic orthostatic intolerance of the postural orthostatic tachycardia syndrome. J Appl Physiol 89:1505-1512, 2000. Abstract. Article PDF.
- Stewart JM, Gewitz MH, Weldon A, Munoz J. Patterns of orthostatic intolerance: The orthostatic tachycardia syndrome and adolescent chronic fatigue. J Pediatr. 1999;135:218–225 Abstract Article PDF
- Benrud-Larson LM, Dewar MS, Sandroni P, et al. Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc 2002;77:531-7. Abstract. Article PDF.
- Raj, S. R., Biaggioni, I., Yamhure, P. C., Black, B. K., Paranjape, S. Y., Byrne, D.W. and Robertson, D. () Renin-aldosterone paradox and perturbed blood volume regulation underlying postural tachycardia syndrome. Circulation. 2005: 111;1574–1582.
- De Becker P, Dendale P, De Meirleir K, Campine I, Vandenborne K, Hagers Y. Autonomic testing in patients with chronic fatigue syndrome .Am J Med. 1998 Sep 28;105(3A):22S-26S.
- Rahman K, Burton A, Galbraith S, Lloyd A, Vollmer-Conna U. Sleep-wake behavior in chronic fatigue syndrome. Sleep. 2011 May 1;34(5):671-8. Abstract. Article PDF.
- Wyller, V. B., Saul, J. P., Walløe, L. and Thaulow, E. Sympathetic cardiovascular control during orthostatic stress and isometric exercise in adolescent chronic fatigue syndrome. Eur. J. Appl. Physiol. 2008: 102;623–632 Abstract.
- Wyller, V. B., Barbieri, R. and Saul, J. P. Blood pressure variability and closed-loop baroreflex assessment in adolescent chronic fatigue syndrome during supine rest and orthostatic stress. Eur. J. Appl. Physiol. 2010: 111; 497–507. Abstract. Article PDF.
- Boneva, R. S., Decker, M. J., Maloney, E. M., Lin, J. M., Jones, J. F., Helgason, H. G., Heim, C. M., Rye, D. B. and Reeves, W. C. Higher heart rate and reduced heart rate variability persist during sleep in chronic fatigue syndrome: a population-based study. Auton. Neurosci. 2007: 137; 94–101. Abstract.
- Newton JL, Okonkwo O, Sutcliffe K, Seth A, Shin J, Jones DEJ.Symptoms of autonomic dysfunction in chronic fatigue syndrome. Q J Med 2007; 100:519–26. Abstract. Article PDF.
Author: Kay E. Jewell, MD
Page Last Updated: August 23, 2012
