Prolonged bedrest can cause Orthostatic Intolerance
Prolonged bedrest results in changes in the cardiovascular system, which includes the heart, the blood vessels, and the hormonal-chemical message systems. This is also called 'cardiovascular deconditioning'. These changes can lead to fast heart rate when the person is resting, a decrease exercise ability and a predisposition to orthostatic intolerance.1,2,
The changes that have been documented in the research include:
- Low blood volume.1,3,5,8
- Decrease in muscle mass1,8, some have reported a decrease in size of the heart3
- Increase responsiveness of the sympathoadrenal system (increase in epinephrine and norepinephrine)1,3,6,7
- Changes in the sensitivity of the baroreceptors (special blood pressure sensor cells in the neck) - changes in its interpretation of the blood pressure and incorrect messages to the body about how to respond.5
- Changes in how the arteries and veins react to low blood pressure3,5,8
The bottom line: The body changes to adjust to prolonged bedrest. This process of adjusting is called "deconditioning". The changes in the cardiovascular system can lead to orthostatic problems. The changes in the muscles can make it harder to recover. To learn more about the body's changes with bedrest, go to Bedrest.
How it all started: People who had a trigger event, like an infection or an accident/trauma often had a prolonged time of bedrest while they recovered. Their body most likely adjusted to the bedrest, it "deconditioned". The body's adjustments to bedrest increased the chance that orthostatic problems would develop or made it worse. There could be other things that happened with the trigger event that also created the problem. However, prolonged bedrest was probably partly the problem.
How it continues: Now that the orthostatic problems are there, a vicious circle gets started. If you get up, decide to "suck it up" and "push through it" ![]() you get more orthostatic stress on the body
you get more orthostatic stress on the body ![]() more fatigue.
more fatigue.![]() That leads to bedrest
That leads to bedrest![]() So you get up and try it again, with more determination this time
So you get up and try it again, with more determination this time ![]() More fatigue
More fatigue![]() More bedrest
More bedrest ![]() More orthostatic problems. It becomes a spiral that only goes down!
More orthostatic problems. It becomes a spiral that only goes down!
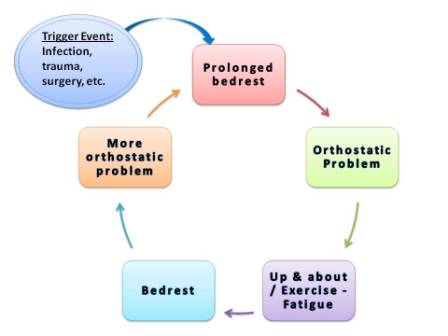
It's time to break the cycle!
We have collected the information you need to manage orthostatic intolerance and the conditions that cause it - Managing OI. There are more details about managing everyday life in the section on Taking Care including Managing Bedrest . Move into Health addresses the physical activity to break the cycle. Deal and Heal provides more information about dealing with OI and creating realistic recovery plans.
References:
- Gazit Y, Nahir AM, Grahame R, Jacob G. Dysautonomia in the joint hypermobility syndrome. Am J Med 2003;115:33-40. Article
- Hasser EM, Moffitt JA. Regulation of sympathetic nervous system function after cardiovascular deconditioning. Ann N Y Acad Sci. 2001 Jun;940:454-68. Abstract.
- Fu Q, Vangundy TB, Galbreath MM, Shibata S, Jain M, Hastings JL, Bhella PS, Levine BD. Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol. 2010 Jun 22;55(25):2858-68. Abstract. Article PDF
- Martel E, Ponchon P, Champeroux P, et al. Mechanisms of the cardiovascular deconditioning induced by tail suspension in the rat. Am J Physiol. 1998;274:H1667–H1673.
- Medow MS, Stewart JM, Sanyal S, Mumtaz A, Stca D and Frishman WH. Pathophysiology, Diagnosis, and Treatment of Orthostatic Hypotension and Vasovagal Syncope. Cardiology in Review 2008;16(1):4-20. Abstract.
- Rowe, Peter. General Information Brochure on Orthostatic Intolerance and Its Treatment. June 2010. Accessed from http://www.cfids.org/webinar/cfsinfo2010.pdf. Accessed May 28.2012.
- Rowe, Peter. Managing Orthostatic Intolerance. Webinar. September 1, 2010. Hosted by CFIDS Association of American. Accessed June 1, 2012. Written material. Slides PDF. Video.
- Winkelman, Chris RN, PhD, CCRN ACNP. Bed Rest in Health and Critical Illness: A Body Systems Approach. AACN Advanced Critical Care: 2009; 20(3); 254-266. Abstract.
Author: Kay E. Jewell, MD
Page Last Updated: September 13, 2012
